Appraisals – Important, but Also Useless…
Appraisals – Important, but Also Useless…

Regular readers will know I have been somewhat triggered by the case of Lucy Letby, the nurse recently convicted of the murder of seven babies at The Countess of Chester. And no, I won’t let it lie. I can’t accept that we either:
a. do nothing b. wait two years for the output of an enquiry, the results of which we could write today.
There are things we can do today. Computers can imagine the unthinkable. Where was clinical Informatics?
Take a look at the chart below:
[/fusion_text]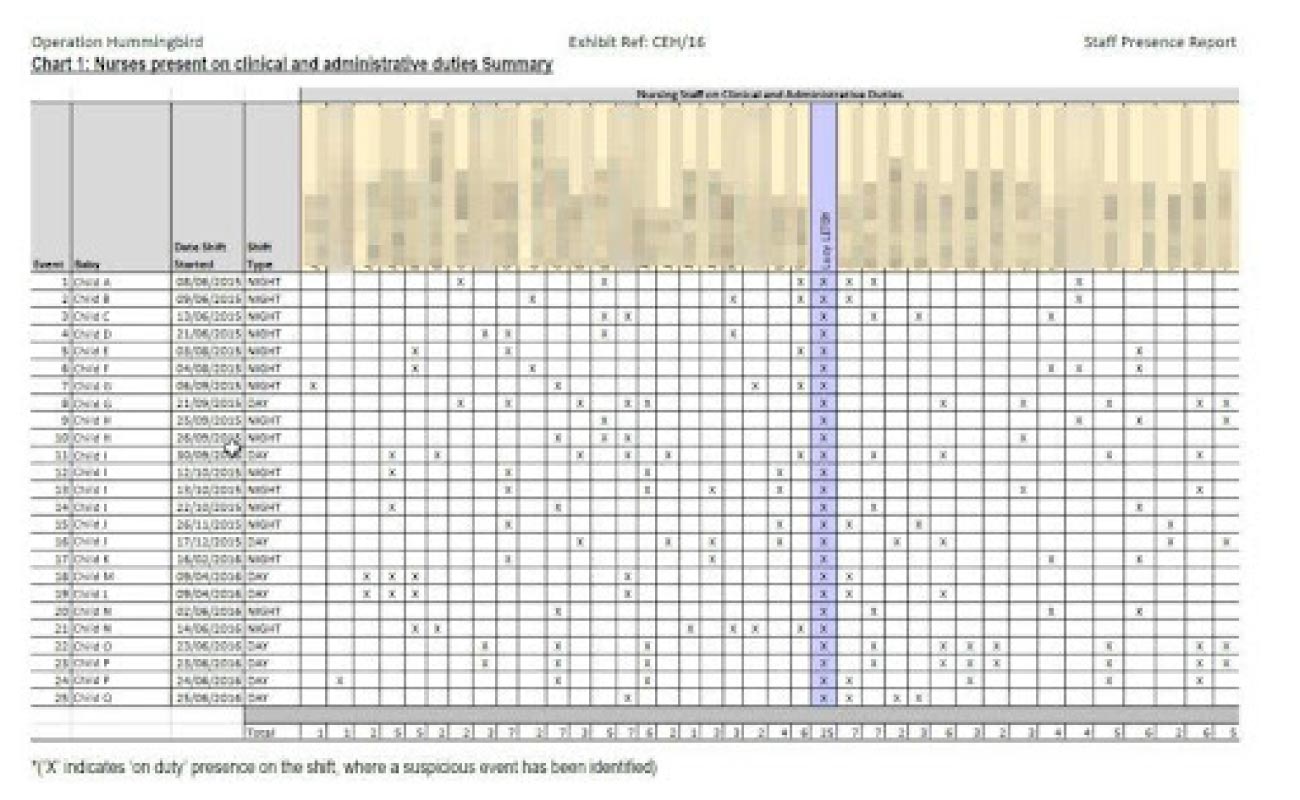
Letby was a massive statistical outlier in terms of her presence during the serious untoward incidents (SUIs) that took place. Surely this could not be ignored? Well it was.
I’m grateful to those who responded to my recent articles on this subject but it’s fair to say I have not been killed in the rush by people wanting to connect the new Patient Safety Incident Reporting Framework (PSIRF) to their annual appraisal. Those who contacted me often pointed out that the Letby case was a failure of organisational culture and management more than a failure of appraisal systems or clinical safety regimes. Fair enough, so we have to address, appraisal, safety systems and organisational culture all at once. Either that or just accept that appraisal of itself is useless from a patient safety point of view and has no place in the prevention of the next Letby/Shipman/Bristol etc.
Appraisal is Useless
I would argue that, in isolation from incident reporting and in the wrong organisational culture appraisal is worthless, just another meaningless paperchase produced by the report into the actions of Harold Shipman. As currently organised appraisal for medics is suboptimal in two major aspects, firstly subjects get to pick the sources for their multisource feedback and secondly they get to choose which , if any, SUIs to bring up at appraisal. Nursing appraisal is even less formalised and appears to have been added as an afterthought and lacks oversight. There is a strong element of lip service in all our current appraisal arrangements.
Can We Fix it?
Yes we can. But it will take a systemic approach and require courage from organisational leadership.
Firstly, appraisal must be for all staff. The post-Shipman response effectively singled out medics for additional scrutiny, the idea that only medics require scrutiny was always fallacious and left the door wide open for Letby.
Secondly, SUI reporting needs to be automatically linked to appraisal systems. Letby’s SUIs should have been fed through a system that alerted an appraiser to her shift pattern/SUI stats which should have spoken for themselves to a dispassionate computer system capable of ‘thinking the unthinkable.’ PSIRF will just be another acronym in a few years time if it doesn’t add some reporting rigour in terms of individual and team accountability.
Thirdly we have to address the cultural issues which often allow NHS patient safety scandals to develop over years without the alarm being appropriately raised. For me there are two elements we could implement immediately:
- Every member of NHS staff should receive training about Professor Cliff Bowman’s Zone of Uncomfortable Debate (ZOUD)* and be encouraged to raise uncomfortable issues in regard to patient safety.
- Every NHS organisation should undertake an assessment of its safety culture. Other safety-critical industries have embraced the assessment of safety culture with tangible improvements in safety. Tried and tested tools exist for the assessment of safety culture in NHS Trusts but are very rarely deployed. The Manchester Patient Safety Assessment Framework (MaPSAF) is an easily deployed cultural assessment process which allows an organisation to assess it’s own safety personality** and address any dangerous cultural issues.
Will We Fix it?
History says ‘no’, but I find that unacceptable. Don’t you?
I’m looking for organisations willing to take bold steps to embrace appraisal and ZOUD training for all, linked to PSIRF and organisational cultural assessment. If you don’t feel you have the internal resources to undertake these tasks please drop me a line and we’ll work something out to get there.
If we aren’t interested in tackling these difficult issues, can we at least stop wasting time on appraisals carried out in a vacuum and time and money wasted on public enquiries that duck the underlying issues? Follow SARD on LinkedIn for more insights and updates.
Prof Joe McDonald, Medical Director
*ZOUD
Regular readers will know I have been somewhat triggered by the case of Lucy Letby, the nurse recently convicted of the murder of seven babies at The Countess of Chester. And no, I won’t let it lie. I can’t accept that we either:
a. do nothing b. wait two years for the output of an enquiry, the results of which we could write today.
There are things we can do today. Computers can imagine the unthinkable. Where was clinical Informatics?
Take a look at the chart below:
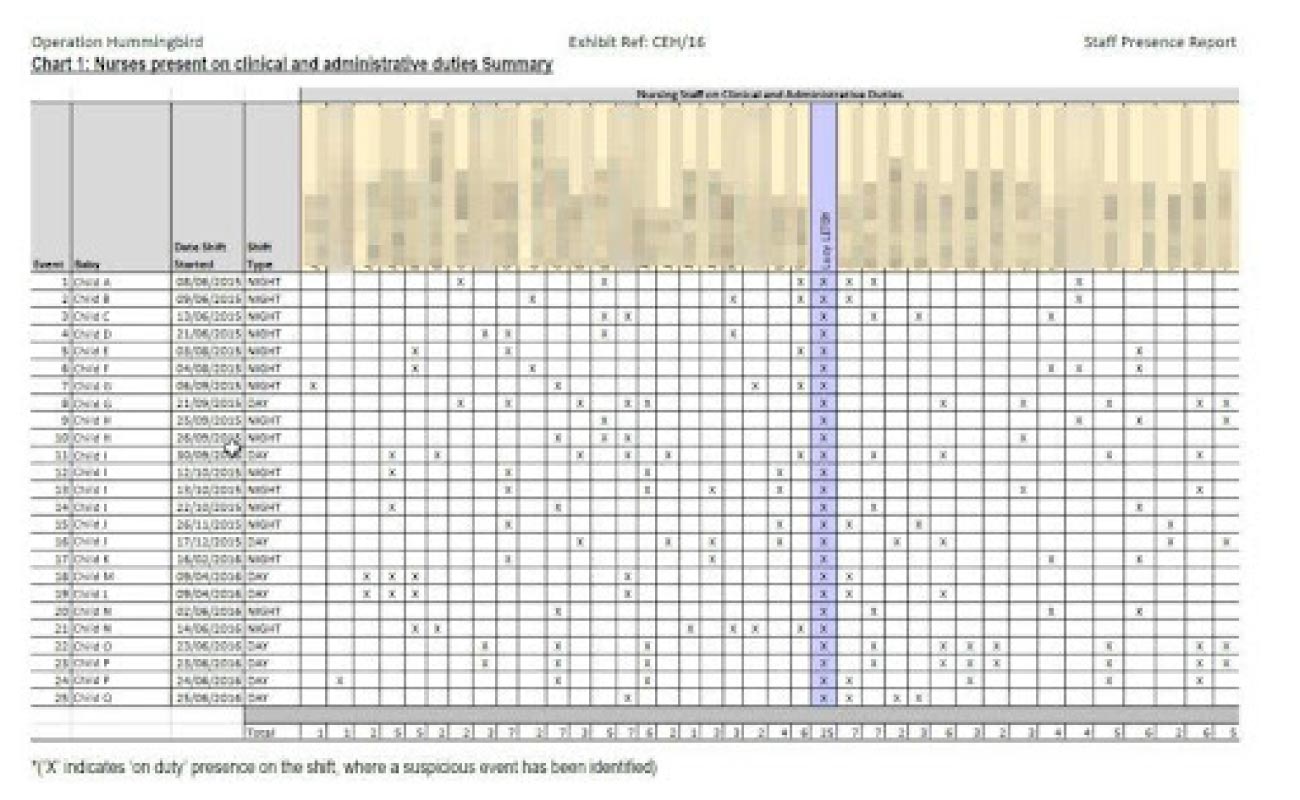
Letby was a massive statistical outlier in terms of her presence during the serious untoward incidents (SUIs) that took place. Surely this could not be ignored? Well it was.
I’m grateful to those who responded to my recent articles on this subject but it’s fair to say I have not been killed in the rush by people wanting to connect the new Patient Safety Incident Reporting Framework (PSIRF) to their annual appraisal. Those who contacted me often pointed out that the Letby case was a failure of organisational culture and management more than a failure of appraisal systems or clinical safety regimes. Fair enough, so we have to address, appraisal, safety systems and organisational culture all at once. Either that or just accept that appraisal of itself is useless from a patient safety point of view and has no place in the prevention of the next Letby/Shipman/Bristol etc.
Appraisal is Useless
I would argue that, in isolation from incident reporting and in the wrong organisational culture appraisal is worthless, just another meaningless paperchase produced by the report into the actions of Harold Shipman. As currently organised appraisal for medics is suboptimal in two major aspects, firstly subjects get to pick the sources for their multisource feedback and secondly they get to choose which , if any, SUIs to bring up at appraisal. Nursing appraisal is even less formalised and appears to have been added as an afterthought and lacks oversight. There is a strong element of lip service in all our current appraisal arrangements.
Can We Fix it?
Yes we can. But it will take a systemic approach and require courage from organisational leadership.
Firstly, appraisal must be for all staff. The post-Shipman response effectively singled out medics for additional scrutiny, the idea that only medics require scrutiny was always fallacious and left the door wide open for Letby.
Secondly, SUI reporting needs to be automatically linked to appraisal systems. Letby’s SUIs should have been fed through a system that alerted an appraiser to her shift pattern/SUI stats which should have spoken for themselves to a dispassionate computer system capable of ‘thinking the unthinkable.’ PSIRF will just be another acronym in a few years time if it doesn’t add some reporting rigour in terms of individual and team accountability.
Thirdly we have to address the cultural issues which often allow NHS patient safety scandals to develop over years without the alarm being appropriately raised. For me there are two elements we could implement immediately:
- Every member of NHS staff should receive training about Professor Cliff Bowman’s Zone of Uncomfortable Debate (ZOUD)* and be encouraged to raise uncomfortable issues in regard to patient safety.
- Every NHS organisation should undertake an assessment of its safety culture. Other safety-critical industries have embraced the assessment of safety culture with tangible improvements in safety. Tried and tested tools exist for the assessment of safety culture in NHS Trusts but are very rarely deployed. The Manchester Patient Safety Assessment Framework (MaPSAF) is an easily deployed cultural assessment process which allows an organisation to assess it’s own safety personality** and address any dangerous cultural issues.
Will We Fix it?
History says ‘no’, but I find that unacceptable. Don’t you?
I’m looking for organisations willing to take bold steps to embrace appraisal and ZOUD training for all, linked to PSIRF and organisational cultural assessment. If you don’t feel you have the internal resources to undertake these tasks please drop me a line and we’ll work something out to get there.
If we aren’t interested in tackling these difficult issues, can we at least stop wasting time on appraisals carried out in a vacuum and time and money wasted on public enquiries that duck the underlying issues? Follow SARD on LinkedIn for more insights and updates.
Prof Joe McDonald, Medical Director
*ZOUD
Recent Articles
Registered address
SARD JV Limited
Unit 76, Innovation Centre
University Road, Canterbury
CT2 7FG
A joint venture with Oxleas NHS Foundation Trust.
Registered in England and Wales with company number 07916735. VAT No. 131901840
Designed and built By Tweak Marketing
Privacy Policy





